Through Module 4 – Comprehending Sexual Health, we enter into the fabulous exploration of bodies: how they work and stay “healthy”. This is a module on the importance of sexual and reproductive health, including prevention of STIs, of unwanted pregnancies and contraception; but also, on body anatomy, in which you’ll find scientific, evidence-based information, enabling to debunk myths and misconceptions surrounding this vital aspect of life.
Voices - Module 4
Introduction
As a young person, the journey of adolescence can be exciting but also challenging. It’s a time of self-discovery, growth and transformation, and part of that transformation involves understanding and taking control of your sexual and reproductive health. According to the WHO:
“Sexual and reproductive health includes a broad range of physical, emotional and social well-being related to your sexuality and reproduction. It does not only cover the topic of preventing unwanted pregnancies and sexually transmitted infections (STIs), but it is also about nurturing healthy relationships, fostering positive body image, and promoting overall well-being” (WHO, 2002).
Sexual health entails a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence, thus going beyond the basic biological processes. The phase of adolescence is a crucial phase for developing a healthy understanding of sexual and reproductive health: acknowledging and embracing sexual health is essential for your overall well-being, as good sexual health positively impacts your self-esteem, mental health and physical fitness. It empowers you in establishing boundaries, and promoting respectful relationships. Moreover, healthy sexual development contributes to building strong foundations for adulthood. Learning about sexual health will enable you to navigate challenges, fostering a sense of responsibility and autonomy. Understanding your own body and knowing how to maintain sexual health empowers you to make informed choices and enjoy fulfilling relationships while, at the same time, reducing potential health risks. However, despite the well-known importance of having a correct understanding of sexual and reproductive health, still various myths and misconceptions surround these topics, leading to confusion and misinformed decisions. Through this module, we will not limit ourselves to offer some accurate and factual information, but instead will unravel some common misconceptions about sexual health.
Key Vocabulary and definitions

Barrier Methods
Medical devices that are commonly available to prevent STIs.
Contraceptive Methods
Medical devices to prevent pregnancies, sometimes available without prescriptions, sometimes needed instead.

Puberty
The moment when “your body goes from being a kid to an adult”: such changes happen overtime, in general between ages 8 and 14.
Sexually Transmitted Infection (STI)
Sexually transmitted infections (STIs) are primarily transmitted through unprotected sexual intercourse, but they can also be spread during pregnancy, childbirth, and breastfeeding, as well as through contaminated blood or blood products.
The most common and curable STIs are trichomonas, chlamydia, gonorrhoea and syphilis. Rapidly increasing antimicrobial resistance is a growing threat for untreatable gonorrhoea.
Viral STIs including HIV, genital herpes simplex virus (HSV), viral hepatitis B, human papillomavirus (HPV) and human T-lymphotropic virus type 1 (HTLV-1) lack or have limited treatment options. Vaccines are available for hepatitis B to prevent infection that can lead to liver cancer and for HPV to prevent cervical cancer. HIV, HSV and HTLV-1 are lifelong infections: for HIV and HSV there are treatments that can suppress the virus, but currently there are no cures for any of these viral STIs.
The term STI has been used in the past years more commonly than STD, since it is more scientifically accurate, and less stigmatising. “Disease” brings a heavy load of stereotypes and negative assumptions (e.g. that it refers to something incurable). Both terms (STD/STI) refer practically to the same thing, but STI is preferred as it is more accurate and less stigmatising connotations.
Genitals
The sexual or reproductive organs located on our body, being internal and external.
Menarche
It is the very first time that people with uterus will get their period. From that time one, a cis girl or a person with a uterus can get pregnant after sexual intercourse. This time is estimated between 11-16 years old.

Menstruation
It happens when blood tissue comes out of the vagina, usually every month. The menstrual cycle is controlled by hormones like oestrogen and progesterone, that make eggs in the overies mature, ready to be fertilised., and make the uterus lining thick for a possible pregnancy. If the egg isn’t fertilised, the thick uterus lining breaks down, and blood and tissue flow out through your vagina. This is the way for your body to tell you that you are not pregnant.
Fertility
It is the ability of an individual to reproduce through sexual activity.
AFAB and AMAB
Assigned Female at Birth and Assigned Male At Birth

Intersex People
Umbrella term describing people born with sex characteristics (including genitals, gonads and chromosome patterns) that do not fit typical binary notions of male or female.

Endometriosis
Endometriosis is a disease in which tissue similar to the lining of the uterus grows outside the uterus. It can cause severe pain in the pelvis.

Vulvodynia
Vulvodynia is prolonged pain in the vulva (area around the outside of the vagina). It does not have a specific cause, and can affect people with vulva of all ages.

Abortion
Intentional termination of a pregnancy, resulting in the removal or expulsion of the foetus. It can be achieved through medical methods (using medications) or surgical procedures.

Healthism
It is the social and cultural belief that implies that your physical, mental and sexual health is your own responsibility, turning the discourse with moral implicit judgments (and prejudices).
Puberty and body anatomy
In this section, we explain the parts into which our genitals are divided and what they are used for. We will start from defining puberty, as the moment when “your body goes from being a kid to an adult”: such changes happen overtime, in general between ages 8 and 14 (AFAB – assigned female at birth – persons often start puberty before AMAB – assigned male at birth – persons do), and quite slowly, not all at once, and more importantly, in very different ways – bodies are unique, as puberty is!
What happens to your body during puberty? This video, created by Planned Parenthood, explains everything about those changes:
“Horrible, I was very ashamed, I hid my hair, I shaved it off, I hid my breasts, especially at home, I was afraid people would love me less because I was no longer a child. It was a very difficult time.”
“Unfortunately, I didn’t have anyone to talk about entering adolescence and I felt very lonely watching my body change”
Puberty affects your body and your emotions, and as all “changes”, may be lived as a stressful, ashaming and confused step: the first advice we would give you is not to worry! Everything is healthy and right. Another tip is to try to find people who you trust and can confide in, whether it’s a close friend, educator or family member, and eventually ask for professional advice – you’ll find some info on this below.
Now let’s see the parts into which our sexual anatomy is divided and their functions:
People with vulva/uterus/ovaries
| Internal | ||
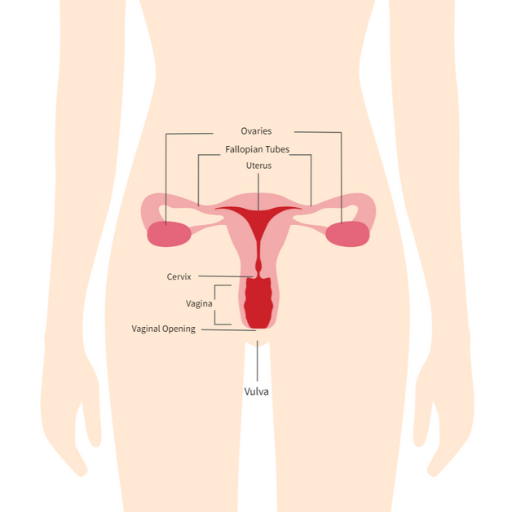 |
Ovaries | These are the gonads in which eggs are produced. They are located in the pelvic cavity on both sides of the uterus. |
| Tubes or Uterine tubes | Muscular tubes that connect the ovaries with the uterus. It is the place where sperm and eggs meet. | |
| Uterus | Hollow muscular organ shaped like an inverted pear, during the cycle menstrual period will be prepared in case an egg is fertilized, as it will move to the uterus where it would be implanted for pregnancy. | |
| Vagina | Muscular tube that connects the vulva to the cervix. As a muscle, we can relax it or put it into tension and this can happen involuntarily. It has an acidic pH during puberty that must be maintained with hygiene routines that prevent alteration of that pH. | |
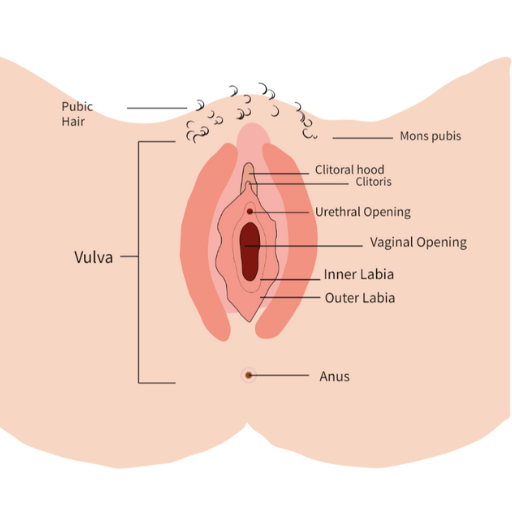 |
External The external organ is called the vulva. It has very different shape, as the organs constituting it:
|
|
Remember that each vulva is unique and that virginity is a social construct! Go and read more about it in module 5
People with penis/scrotum/testicles
|
Internal |
||
|
|
Testicles |
2 ball-like glands inside scrotum. They make sperm and hormones like testosterone. |
|
Epididymis |
A tube where sperm matures. It connects each testicle to each vas deferens. And it holds your sperm before you ejaculate (come). |
|
|
Vas Deferens |
Long, narrow tube that carries sperm from the epididymis to the seminal vesicles when you ejaculate (come). There are 2 of them — one connected to each epididymis. |
|
|
Seminal Vesicles
|
2 small organs that produce semen, the fluid that sperm moves around in. They’re located below your bladder. |
|
|
Prostate Gland |
It makes a fluid that helps your sperm move. It’s about the size of a walnut or golf ball. The prostate gland is sensitive to pressure or touch in a way that many people find pleasurable. |
|
|
Cowper’s glands |
They produce a fluid called pre-ejaculate or precum. This fluid prepares your urethra for ejaculation (coming). It reduces friction so your semen can move more easily. The Cowper’s glands are under the prostate and attach to your urethra. They’re also called bulbourethral glands. |
|
|
Urethra |
The tube that carries urine (pee), pre-ejaculate, and semen to your urethral opening and out of your body. |
|
|
Cremaster |
A muscle that moves your scrotum and testicles closer to your body. This happens when you’re cold, you’re aroused, or when someone touches your inner thigh. |
|
|
External |
||
|
|
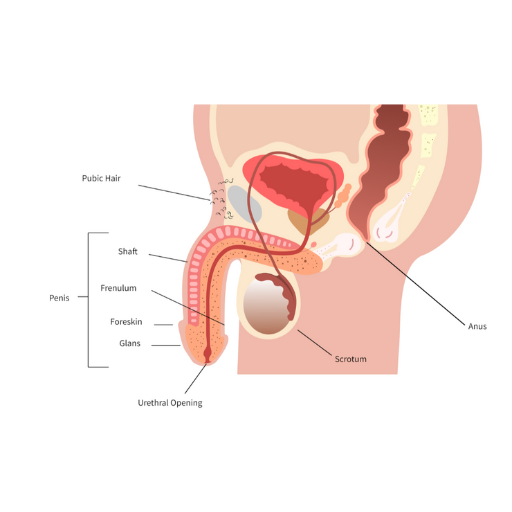
Penis |
Organ through which urine, seminal fluid and semen are expelled. It is divided into several parts: ● Glans: also called the head or tip of your penis. The opening of your urethra is here. This is where pre-ejaculate (precum) and semen (cum) come out of, and it’s where you pee out of. For many people, it’s the most sensitive part of the penis. ● Shaft: it extends from the tip to where it connects to your lower belly. It looks like a tube. Your urethra is inside the shaft. ● Foreskin: a patch of skin that covers and protects the head. When your penis gets hard, the foreskin pulls back and the tip is exposed. Sometimes foreskin is circumcised (when a doctor surgically removes your foreskin) soon after birth, so not everyone has it. ● Frenulum: where your foreskin meets the underside of your penis. It looks like a small V just below the head. Usually part of it remains after circumcision. And for many people, it’s very sensitive. |
|
Scrotum |
The scrotum (or ballsack) is the sac of skin that hangs below your penis. Your scrotum holds your testicles and keeps them at the right temperature. If it’s too cold, your scrotum pulls your testicles closer to your body. If it’s too warm, your testicles hang away from your body.
Your scrotum is covered with wrinkly skin and hair. Your scrotum can be big or small, have a little or a lot of hair, and vary in color. Some people’s scrotum is larger on one side than the other.
The scrotum is super sensitive, so any hitting or twisting is extremely painful. But many people like having their scrotum gently touched during sex. |
|
|
Anus |
The anus is the opening to your rectum. The anus has lots of sensitive nerve endings, so some people experience sexual pleasure from anal stimulation. |
|
Intersexuality and anatomy
Genitals and sexual characteristics can have some variations: we are talking about intersex people. They can have variations of chromosomes, hormone levels, genitalia (ambiguous genitalia).
Some can be:
- Congenital adrenal hyperplasia (CAH): XX individuals with “masculinized” genitalia, “masculine” characteristics at puberty;
- Androgen Insensitivity Syndrome (AIS): XY individuals with “feminised” genitalia, can develop “feminine” body shape;
- Turner Syndrome: only X chromosome (XO)
- Klinefelter Syndrome: extra X chromosome (XXXY)
According to some studies (vd. Anne Fausto Sterling) intersex people are 1,7% of the population – it’s almost the same percentage of people with red hair in the world! Sometimes they don’t have a “diagnosis” until adulthood, sometimes a diagnosis is made because some condition brings infertility. An intersex person may have any gender identity (see module 2).
In most countries intersex people are assigned at birth to one or other sex (M/F).
A very important topic for the LGBTQIA+ community and specifically the intersex community is the topic of genital surgery on intersex people: in many countries, surgical operations are performed on newborns to make the genitals more similar to a vulva or a penis, in order to assign a sex to the person. This is problematic because the person did not have a choice and often this surgery is not performed for health issues.
Intersex conditions are variations of the cultural binary, not a disease, although some conditions could cause syndromes and discomfort, there are a huge number of different sex characteristics.
Anatomy of people with vulva and pleasure
Anatomy of people with vulva and acknowledgment on how their genitalia works have been a mystery for decades and still today there is a gender gap in medical and health research, with consequences on women and people with vulva sexual health and knowledge around female pleasure.
In 2005 the Australian urologist Helen O’Connell studied and discovered the full anatomy of the clitoris, the organ whose function is entirely meant for giving pleasure. The results of her study “Anatomy of the clitoris” (O’Connell et al., 2005) showed that the typical textbook descriptions of the clitoris didn’t provide detailed information about this organ and also included inconsistencies. Helen O’Connell discovered that the whole clitorial cluster, made of really sensitive erectile tissue, is the key to sexual function and orgasm of people with vulva. Also: there are more similarities between the structure of the clitoris and the structure of the penis than differences; that’s not only interesting, but it also points out how scientific progress could have been done simultaneously in the medical and wellness fields, being neglected and biased by gender discrimination instead.
From this point on, social, political and medical discussion have taken new directions about sexual wellness and pleasure, highlighting the obscurantism based on gender discrimination for women and people with vulva.
What about self-exploration? Differently from the penis, the vulva is also harder to explore. It is located on the body in a way that requires the use of a mirror and or a speculum. In addition, due to patriarchy, women have been sexually censored by society for ages, in a way that affected their freedom to explore it and get to know it as a source of pleasure, or live their enjoyment without fear, shame or guilt. Still today there is great ignorance around female pleasure and many cisgender women and people with vulva rarely reach the orgasm. Heterosexual cisgender women are the ones that have less orgasms of all: only in 65% of cases.
Now we’re seeing a wider public discourse that centres pleasure, personal experiences and preferences, adding nuances and in-depth analysis on sexuality that move away from phallocentrism and gender invisibilization.
Menstruation
A term not well-known is menarche. This is the very first time that people with uterus will get their period. From that time one, a cis girl or a person with a uterus can get pregnant after sexual intercourse. This time is estimated between 11-16 years old.
In order to understand how this process starts and continues for people with uterus, we need to examine menstruation. Menstruation, in common terms “period”, happens when blood tissue comes out of the vagina, usually every month.
Your menstrual cycle is controlled by hormones like estrogen and progesterone. In simple terms: You have 2 ovaries, each with tiny eggs. Hormones make the eggs mature, ready to be fertilised. They also make the uterus lining thick for a possible pregnancy. Midway through your cycle, hormones trigger ovulation, releasing a mature egg. You might feel bloated or in some pain. If the egg isn’t fertilised, the thick uterus lining breaks down, and blood and tissue flow out through your vagina. This is the way for your body to tell you that you are not pregnant.
Be careful though! Having your period does not mean that you cannot get pregnant. Ovulation typically occurs approximately 14 days before the onset of your period, though individual bodies vary. The timing may be earlier or later based on the length of your menstrual cycle. Once released from the ovary, an egg survives for about 1 day, while sperm can persist in the uterus and fallopian tubes for approximately 6 days after intercourse. This means there’s a potential window of around 6 days in each menstrual cycle during which pregnancy can occur. In order to be prepared about your menstrual cycle, you can keep track of your ovulation days on apps or in a calendar. Of course, when the time comes, it is important that you are equipped with period products to absorb the blood flow, like pads, tampons and reusable panties and cups.
Girls, trans boys, nonbinary people and other people who menstruate don’t receive adequate information prior to their menarche! Also, the message that is transmitted to the girls and other menstruating people is that once the period arrives, they are not girls or kids any more, but grown-ups. This idea totally disorients them as it seems that their personality should change at the drop of a hat, with all of those behaviours that were accepted just before menstruation are no longer correct. Also, while it is a fact that the menarche determines the beginning of fertility, it is very common to hear a discourse exclusively based on the fear of an unplanned pregnancy.
In this sense, CSE along with menstrual education ensure that menstruating young people receive all the information on:
- the available products to manage their bleeding;
- the implications that becoming cyclical has for the physical, emotional and sexual well-being;
- the considerations to take into account regarding cyclicity and fertility so that each one achieves the highest level of body awareness, self-knowledge and empowerment.
What is also important to recognise is that menstruation is nothing to feel embarrassed about but rather something to be prepared for. Periods can be experienced way differently by each person. Symptoms like pain cramps, muscle pain and mood swings are quite common. Feel free to cry, get cozy with warm blankets or exercise during your period cycle. There are times that people with vulva will experience excessive pain or other symptoms that cannot be directly connected to your period. Do not worry, you are not alone! Worldwide, 26% of people with a vulva has chronic intimate pain and suffer from the so-called “silent illnesses” that cause them such pain or other symptoms, such as excessive blood flow, and may makes life very hard interfering with the most simple everyday activities, such as having sex or working at full strength, impacting physical and mental health. One of these silent illnesses is endometriosis: according to statistics, 1 out of 5 people with uterus have it, but it takes up to 8 years for a person with uterus to be diagnosed with endometriosis. A common symptom is pain in the lower part of the belly (pelvis). Pain may be most noticeable: during a period, during or after sex, when urinating or defecating. In some other cases, there are no clear symptoms and the diagnosis arrives by chance.
Another silent illness is vulvodynia. As the name of the illness reveals, vulvodynia is causing unexplained pain in and around the vulva. Some steps you can follow in order to reduce the symptoms are the following:
- Opt for cotton underwear and loosely fitting skirts or pants.
- Steer clear of scented hygiene products, including feminine wipes, bubble bath, and soap;
- Alleviate discomfort by applying chilled gel packs to the vulva.
- If sexual activities are something you want to do, it may be useful using a water based lube (be careful because a lot of lubes are not good for your genitals, ask an expert!
- Prior to swimming, apply petroleum jelly to shield the vulva from chlorine.
- Avoid completely or vulva touching, as it may heighten sensitivity.
- If intercourse is painful, explore more comfortable positions or engage in alternative intimate activities until seeking advice if penetration remains painful.
- Work on reducing stress, as it can amplify vulvodynia-related pain.
- To ease sitting discomfort, use a cushion with a doughnut-shaped design.
Experiencing pain is not normal!
In case you have symptoms that do not make sense to you, speak about it with your doctor, as soon as possible!
Do you want to learn more on genito-pelvic pain?
“My first contacts with sexual health were due to medical needs, because I had an operation for endometriosis and had to go to the gynaecologist, but by then, at 22, I had already developed and even had sex for a long time and nobody had asked me to go to the gynaecologist. On my own I had searched for information about family planning consultations and went to some information sessions to get the best (and most effective) contraceptive.”
Abortion
Abortion is the intentional termination of a pregnancy, resulting in the removal or expulsion of the foetus. It can be achieved through medical methods (using medications) or surgical procedures. Contrary to what it could be considered, abortion has not to be a traumatic experience and access to safe and legal abortion services, as well as supportive healthcare and counselling, is crucial for people with uterus’ reproductive rights. Here’s the different methods:
- Medical: Involves the use of medication to terminate a pregnancy. Typically, a combination of drugs, like mifepristone (a drug that blocks progesterone) and misoprostol (a drug that induces uterine contractions to expel the pregnancy). Usually performed within the first 10 weeks of pregnancy; effectiveness is high.
- Surgical: Involves a procedure to remove the pregnancy from the uterus, for example: suction aspiration (done by a sort of little tube inserted in the uterus to which a valve pumps the air in that creates a suction to remove the tissue), or dilation and curettage (D&C) (the cervix is dilated and the “curette” – a sort of spoon-shaped tool – is inserted in the uterus to remove tissue). Surgical methods could be performed in different stages of pregnancy but it strongly depends on legislative regional laws.
Following the data given by reproductiverights.com, there are 5 main categories in which laws concerning abortions are developed:
On request
Abortion is permitted on request, although each country has different laws concerning gestational limits, which are calculated from the first day of the last menstrual period, which is considered to occur two weeks prior to conception. Where laws specify that gestational age limits are calculated from the date of conception, these limits have been extended by two weeks. Among countries that adopt this category are: Albania, Argentina, Armenia, Belgium, Benin, Bosnia & Herzegovina, Finland, France, French Guiana, Georgia, Germany, Greece, Italy, most European countries, Turkey, Vietnam and many more.
Broad social and/or economic grounds
Abortion is available on broad social and economic grounds that take into account the pregnant person’s situation, economic circumstances, and well-being. Among the countries: Barbados, Belize, Ethiopia, Fiji, India, Japan and many more.
To preserve health
Abortion is permitted when pregnancy poses a risk to the person’s health. Among the countries: Algeria, Angola, Bolivia, Burkina Faso, Costa Rica, Democratic Republic of Congo, Ecuador, Kuwait, Namibia, Zimbawe and many more.
To save a pregnant person’s life
Abortion is allowed in certain specific grounds, such as when pregnancy results from rape or incest or in cases of certain fetal diagnoses. Among the countries: Afghanistan, Bangladesh, Chile, Dominica, Gabon, Indonesia, Iran, Lebanon, Libya, Malawi, Myanmar, Nigeria, Palestine, Panama, Somalia, Sri Lanka and many more.
Prohibited altogether
Abortion is forbidden. These are the most restrictive abortion laws in the world. Among the countries: Andorra, Congo, Dominican Republic, Egypt, Haiti, Iraq, Jamaica, Laos, Madagascar, Nicaragua, Philippines, Senegal, Tonga and many more.
Sexually transmitted infections (STIs)
“We do not receive any information on the topic of sexual health: in my culture it is a big taboo that is forbidden to talk about. I am finding out today that there are sexually transmitted diseases.”
Sexually transmitted infections (STIs) are primarily transmitted through unprotected sexual intercourse, as well as through contaminated blood or blood products and they can also be spread during pregnancy from the pregnant person to the foetus, childbirth, and breastfeeding. The term STI has been used in the past years more commonly than STD, as “disease” brings a heavy load of stereotypes and negative assumptions (e.g. that it refers to something incurable), and above all may be not correct at all in some cases (e.g. HIV is different from AIDS).
Common Sexually Transmitted Infections (not exhaustive list)
Chlamydia
A bacterial infection caused by the bacteria called “chlamydia trachomatis”. Most people with penis and people with vulva don’t have symptoms of it but can lead to serious complications if left untreated; it can be passed through oral sex and penetrative sex (anal and/or vaginal) because it can be passed through body fluids. Treatment can be done with antibiotic cure.
Gonorrhea
A bacterial infection caused by the bacteria “neisseria gonorrhoeae”. Sometimes there are no symptoms, however gonorrhoea distinguishes various symptoms between people with penis and people with vulva:
-
- for people with penis: yellowish-white discharge from the penis, burning or pain when urinating, urinating more often than usual, pain or swelling of the testicles;
- for people with vulva: abnormal discharge from the vagina that is yellow and sometimes bloody, burning or pain when urinating.
It can affect the genitals, rectum (anal zone), and throat. Gonorrhoea can be treated with injection of antibiotics.
Hepatitis
An inflammation of the liver that can be caused by a group of viruses. There are five major types of viral hepatitis: hepatitis A, hepatitis B, hepatitis C, hepatitis D, and hepatitis E; Hepatitis A, hepatitis B and hepatitis C are the most common types of viral hepatitis. Although many cases of hepatitis are not a serious threat to health, the disease can sometimes become chronic (long-lasting) and may lead to liver failure and death. Here following some insight on Hepatitis A and B for what there’s a vaccine to prevent them.
Hepatitis A
Is transmitted primarily through oral contact with faeces (oral-faecal contact). This includes contaminated food or water sources and sexual contact, especially oral-anal sex. Some symptoms include: low-grade fever, fatigue, loss of appetite, nausea, abdominal discomfort, dark-coloured urine, jaundice (yellowing of the skin and the eye). Once recovered, an individual is immune and will not get hepatitis A again. Many countries provide vaccination against Hep A, sometimes for free.
Hepatitis B
Is passed on through contact with infected body fluids such as semen, vaginal secretions, and blood. It is most often transmitted through sexual contact but can also be contracted when injecting drug users share needles and other injecting equipment. Mothers with hepatitis B can also pass the virus to their infants during birth. Hepatitis B is not spread through food, water, sharing utensils, hugging, kissing, or by casual contact.
Some symptoms include: acute infection causing mild illness for a few weeks or months, more serious chronic infection lasting a lifetime. Hepatitis B is preventable through vaccination. A person can choose to be vaccinated and no longer have to worry about being infected with hepatitis B (many countries provide mandatory and free vaccination against Hep B). In many cases, though, viral hepatitis is a self-resolving illness—meaning it goes away on its own. As regards another serious type of hepatitis, hepatitis C, it is important to remember that it is transmitted mainly through blood (micro-lesions during sexual intercourse can transmit the virus). It can be very dangerous, but there are medications to treat it.
(Genital) Herpes
Oral herpes (also known as HSV, “herpes simplex virus”, that one around the mouth, sometimes called cold sores or fever blisters) can be passed on through kissing or oral sex. If a person with oral herpes performs oral sex, it is possible to pass along the infection to the partner’s genitals. If a person with genital herpes has sex, it is possible for their partner(s) to get genital herpes. Any person who is sexually active can get genital herpes. Some of the symptoms are the “lesion” in the skin of the interested area: sores, vesicles or ulcers; genital herpes resemble small pimples that crust over, eventually; sometimes happens also headache and painful urination due to the ulcers in the sensitive part of the genitals. Mostly approved treatments for Herpes are antiviral pills to be prescribed, but the infection stays latent in the body and can cause symptoms again.
HIV
“HIV” stands for “Human Immunodeficiency Virus”; it’s the virus that causes AIDS (“Acquired Immune Deficiency Syndrome”). HIV (which is the virus) once in the body infects cells of the immune system, impairing their function: AIDS is the disease that comes when the immune system is compromised.
HIV could be transmitted via blood, sexual fluids (semen, vaginal fluid) or breast milk of an HIV- infected person; could be passed through unprotected penetrative sex, vaginal and/or anal, but also via using the same shared needle when doing injections, if one of the people involved has HIV.
HPV
“Human Papillomavirus” is a name of a group of viruses that could infect the body. There are over 100 different types of human papillomavirus, or HPV. Some types of HPV can cause genital warts and other types can cause cancer, including cancer in the genital zone, external and internal (vagina, vulva, penis, anus and rectum). The lower risk type of HPV could cause the genital warts; the higher risk types cause the cancer.
Hpv is very common, whoever has a sexually active life could contract the virus at some points: it is spread through direct skin-to-skin contact (so of course genital contact included) with someone who has any sort of infection.
In most cases, HPV is pretty harmless: the body reacts and cleanses itself autonomously. But as mentioned before, there are certain types that can cause cancer, that’s why a regular screening is highly suggested.
There is a vaccination to prevent HPV infections: getting vaccinated from the age of 9 years old is highly recommended for every person regardless of their gender.
Syphilis
It is a bacterial infection caused by “Treponema pallidum”. Syphilis is passed on when infected lesions (like bruises, scratches, little cuts in the skin) come in contact with the genital zone, both internally (vagina, urethra, anus) and externally during oral sex, even if there is no sexual penetration.
There are 4 stages through which untreated syphilis progresses, each stage with its own unique signs and symptoms: primary, secondary, latent, and tertiary (or late). In summary: the primary stage is characterised by the so-called “chancres” (basically a single sore that appears outside or inside the genitals, most of the time painless). Chancres can go away without treatment although passing away without medication could mean that the infection is still there; in the secondary stage symptoms are: reddish-brownish rash peculiarly on the palms of your hands or in the soles of your feet, as well as in other parts of your body; moist and elevated skin lesions could be found in the genital area, anus included; greyish sores in the mouth and in the throat and a generally sense of ill health. As well as the primary, also in the secondary all the symptoms could go away without treatment but always with the risk of the infection still being there.
Latent stage: as the name suggests, there’s no clear symptoms in this stage and the only way to know is to take a blood test. The tertiary or late stage have symptoms that could take from 2 to 30+ years after infection. Complications could be: so-called “gummas”, small bumps or tumours developed on the skin, on the bones and other organs; cardiovascular problems and chronic nervous system disorders.
If treated on time gummas will disappear, curing the disease and avoiding future damages, but it cannot reverse the damages already done, if appeared.
To treat syphilis: penicillin is highly suggested and preferred, but if you are allergic to penicillin, your healthcare provider can suggest another antibiotic.
Trichomoniasis (also known as “trich”)
Is a common, curable STI caused by a parasitic protozoa called “Trichomonas vaginalis”. As you can sense by the Latin name, is an infection that affects people with vagina with clear symptoms.
Trich is spread through sexual contact with an infected partner: this includes penis-to-vagina intercourse or genital-to-genital contact.
Symptoms are: green, yellow or grey vaginal discharge; a bad vaginal smell; itching inside or around vulva and vagina; pain during sex and during urinating.
Most people with penis don’t have symptoms but when it happens it’s about an itching inside or around the penis, a discharge or pain during urinating. Generally, symptoms could be there or not, but without treatment the infection could last months or even years.
To have Trich diagnosed: the parasite it’s harder to detach in people with penis and surely waiting for the symptoms isn’t enough, as we saw they do not always appear. For people with vagina it’s important to book an appointment when monthly periods have ended and if they have less than 24 hours before the exam.
Treatments: with antibiotics typically metronidazole (Flagyl) or Tinidazole (Tindamax).
Talk to professionals, but also to your partners!
about the different barrier methods (see section below), the possibilities of vaccination, and measures such as PREP/PEP
PrEP stands for “Pre Exposure Prophylaxis”; “prophylaxis” itself means to prevent and/or control the spreading of infections or diseases. Specifically, with PrEP the prevention concerns HIV (see the paragraph above) to avoid the infection taking hold if someone gets exposed. There are two ways of taking PrEP:
- Oral PrEP is a pill to be taken daily to prevent HIV infection in someone who’s HIV- negative. When taken consistently, results have shown that PrEP effectively reduces the risk of HIV infections in people who are at high risk.
- PrEP injection has to be administered every two months.
People who are on PrEP are advised to follow up and get tested for HIV every 3 months, that means that it’s not just the medication itself, but also a continuous monitoring for your personal health.
“PEP” stands for “Post Exposure Prophylaxis”; the concept is similar to the PrEP but as you may notice by the name “post” is a medication to be taken after a risky exposure. PEP is for people who have possibly been exposed to HIV. It is only for emergency situations: you should take this as a pill within 72 hours after a possible exposure to HIV. PEP is only for emergency situations. It is not the right choice for people who may be exposed to HIV frequently – for example, if you often have sex without a condom with a partner who is HIV-positive.
Both PrEP and PEP are barrier methods but only for HIV infection, as they’re treatment to avoid HIV from spreading. They do not protect from other STIs (from which you can protect anyway by monitoring via PrEP procedures, that actually require exams every 3 months) and they do not prevent unwanted pregnancy.
Test yourself!
Although some people might have symptoms of a STI, in many instances STIs have no visible symptoms. The only way one might know that they have STIs is through testing!
Treat, with no fear
If you test positive for an STI, don’t worry: all STIs are treatable.
Other suggestions:
- Use lubricants (be aware that not all lubes are ok for condoms, water based and silicon based are ok)
- If sex toys are involved and shared with partner, is important to put a condom on or cleaning it: sex toys can be vehicle of STI
Barrier methods and Contraception
While terms “safe sex” and “safer sex” are used interchangeably, it is nowadays more accurate to use the latter. Any sexual intercourse entails a risk and thus, there is no 100% safe sex. Also, the term “safe sex” can lead to a misconception and avoidance of communication between two (or more) sexual partners. There is a difference between barrier methods and contraceptives: the first are all those medical devices that are commonly available (you can find them in shops and supermarkets without a medical prescription) to prevent STIs (sexually transmitted infections); the latter are medical devices to prevent pregnancies, sometimes available without prescriptions, sometimes needed instead. Sometimes the two categories overlap, meaning that what works as a barrier method also protects from pregnancies, doing both preventive and contraceptive methods.
List of the most common barrier methods and contraceptives
Condoms: condoms are membranes of different materials (latex, polyurethane, polyisoprene) that act like a barrier around or inside genitals. They are distinguished in two categories:
- External condoms: commonly known as “male condoms” are those meant to be worn by people with penis; they can be made of different materials (also hypoallergenic), different sizes, different colours, different flavours…
- Internal condoms: commonly known as “female condoms” are those meant to be worn by people with vagina.
While external condoms could be worn in a few moments before the sexual intercourse, internal condoms could be worn even some hours before; as the internal condoms must fit the vaginal canal, you can differentiate them from the external ones because they are stored in a singular bigger pack.
You can find external condoms mostly everywhere: drugstores, shops, supermarkets and their cost is pretty much affordable. Unfortunately, we can’t say the same for the internal ones: they are difficult to find and their cost is unfairly high; you can find them online and via some drugstore probably with a specific order required.
Every condom, external or internal, must be used once per sexual intercourse: they are disposable and you can’t use it the same, multiple times.
You should be careful about possible allergies due to the material and choose wisely which condom is proper for your health. Condoms are both a barrier method and contraceptive as they are meant to contain semen and other body fluids to avoid sexually transmitted infections and risk of unwanted pregnancy.
- Dental dam/ oral dam: the dental dam, also called “oral dam” is a latex rectangular used for practising oral sex safely: you just have to put on the genital or anal area you’re going to stimulate to use it as a barrier to avoid STIs. Dental dam is just a barrier method. Since it’s not always easy to find, it can be “made” by cutting a condom in half.
Birth control pills: birth control pills are oral contraceptives to take in order to inhibit ovulation and thicken cervical mucus (see menstruation paragraph), typically estrogen or progestin. That means that these pills act like a suspender for the fertility phase of the menstrual cycle. Birth control pills have to be prescribed by a healthcare provider after some texts to understand which kind of pills suit you better according to your health situation and benefits. Birth control pills are contraceptives, not a barrier method: they do not protect from STIs.
In some countries, hormonal contraceptive pills are prescribed to be taken for three weeks consecutively, followed by a one-week pause to coincide with menstruation. The pause week, often referred to as a “withdrawal bleed“, mimics a menstrual period but is not biologically necessary. Modern research suggests that continuous pill use without a pause may be equally safe and effective, reducing the risk of unwanted pregnancies associated with the pause week. Let’s check the main differences between the two methods:
Birth control pill with “withdrawal bleed pause”:
- Taken for 21 days consecutively.
- Followed by a 7-day pause for a withdrawal bleed (mimicking a menstrual period).
- The pause is a traditional practice influenced by historical and cultural factors.
- During the pause, hormonal levels drop, leading to a withdrawal bleed.
Birth control pill as a continuous taking:
- Eliminates the withdrawal bleed and continuous hormonal levels are maintained.
- Reduces the risk of missed doses during the pause week, enhancing contraceptive reliability.
- May offer benefits such as reduced menstrual symptoms and pain.
- Equally effective in preventing pregnancy compared to cyclic use.
Some cultural traditions and early contraceptive pill formulations influenced the first pattern, more rooted in historical practices and cultural beliefs (see module 5) rather than medical necessity. Up to now, the second one is largely supported by progressive medical practices and research; nonetheless the choice depends on individual preferences.
Emergency pill (morning-after pill): as you can assume by the name, this pill is the one you take after having unprotected sexual intercourse and you’re at risk of unwanted pregnancy; it could happen you need to take one of them because condoms broke or you or your sexual partner forgot to the daily birth control pill. This pill is most effective when taken as soon as possible after unprotected intercourse: can be taken up to 72 hours (some types up to 120 hours) after unprotected sex. It works the same as the birth pill, so its function is to inhibit the ovulation and delay all the menstrual cycle as it commonly goes. If you’re a person with uterus you may want know this: both birth control pills and emergency pill influence your menstrual cycle in a way that could feel a little discomfort in the beginning: since they both work on delaying ovulation, everything in your menstrual cycle adapt to the changes and reset, that means that your periods could anticipate or come be late according to your original habits. This is nothing to panic about, just consider consulting your trusting health provider to choose what’s best for you. As birth control pills, this pill is contraceptive, not a barrier method: it does not protect from STIs.
Contraceptive patch: it’s literally a patch, waterproof, you can put on your body, typically on the abdomen, it works via hormones absorbed by the skin, it releases estrogen and progesterone. It also acts on the menstrual cycle the same way birth control does. A new patch is applied weekly for three weeks, followed by one week without a patch. You need a prescription to start using it and it does not protect you from STIs.
Contraceptive ring: is a flexible ring meant to be inserted in the vagina and it releases hormones to delay ovulation. You can insert it autonomously and it has to be changed every three weeks plus a suspension week (you don’t have to put it on while having your period, and you can replace a new one when periods end). Also need a prescription and neither does it protect you from STIs.
Intrauterine device (IUD): it’s a small, T-shaped device inserted into the uterus by a healthcare professional to avoid unwanted pregnancies (it does not protect from STIs). There are two types:
- Copper IUD: it has no hormones, it releases copper that creates an unhospital environment for sperms; it is effective up to 10 years.
- Hormonal IUD: it releases progestin, inhibits ovulation, thickens cervical mucus, and alters the uterine lining. It is effective for up to 3 to 7 years.
IUD is immediately effective as contraception after insertion; up to now there is no rate of inefficiency. It is suitable for people with uterus that want a long-lasting contraception and it is reversible, meaning that whenever someone decides to interrupt this contraceptive method it is possible to.
Contraceptive implant: is a flexible plastic rod placed under the skin of the arm. The implant releases hormones, and it lasts at least 3 years. It’s reversible.
Permanent contraceptive Methods: permanent contraceptive methods are those chosen to avoid unwanted pregnancy permanently (they do not protect from STIs). There are mainly two types and both of them are surgical interventions.
Tubal ligation: for people with uterus. It consists in a surgical sealing of the fallopian tubes. It prevents the fertile egg from travelling through the fallopian tubes to meet the sperm. Once choosing these contraceptive methods, there is no need for other kinds of methods.
Vasectomy: for people with penis. It consists in a surgical blocking of the vas deferens, the tubes that carry sperm.
These are the most common barrier methods and contraceptive methods you will find around. But there are also other elements to consider while thinking about safer sex:
- Ensure that both you and your partner provide consent for sexual activity and have the opportunity to communicate about what brings pleasure.
- Talk and share about your boundaries and what you want to do and what you don’t.
- If you meet someone with HIV, there is no need of panic, do not give up of common stigmatisation: if the person is on HIV treatment, there is the U=U rule:
- U=U stands for undetectable = untransmittable: when a person with HIV has an undetectable viral load thanks to antiviral treatment, it means that they can’t pass the virus. This means that whoever has HIV can still have a regular sexual life if starting as soon as possible with antiviral treatment, for them and their(s) partner(s).
- Taking responsibility for your and your partner’s well-being through safer sex practices allows you to fully savour the pleasures that sexual intimacy can bring.
- Some countries provide some (or all) contraceptive for free at certain ages or to everyone. Talk to the nearer healthcare point!
Myth: Oral sex is safe sex
Fact
Some STIs can also be transmitted through oral sex. So oral sex cannot cause pregnancies but some common STIs can also be transmitted through oral sex such as chlamydia gonorrhoea, herpes and hepatitis.
Sexual Health as a taboo
“I learned sexuality on my own and in a more mature stage sharing it with my friends, during puberty I could not share with anyone those changes and I felt very bad.”
There is a reason that is still very alive today turning sexual health into a taboo: lack of education. Unfortunately lack of education can also lead to psychologically harming consequences such as stigmatisation. Stigmatising sexual health can render couples and other partners in different types of relationships (see module 2 of this guide) to find it difficult to discuss their desires, boundaries, and concerns, which can lead to misunderstandings and dissatisfaction.
The ways stigma surrounding sexual health can be detrimental are multiple:
- On one hand it takes the shape of taboo, excluding every discourse about safety and STIs from the table: absence of CSE about sexually transmitted infections make difficult to people interested in sexual intercourses to have acknowledge and discuss privately about how to have sex, which preventive method and contraceptive to use, what they prefer and what they want to experience;
- On the other hand, focusing just on STIs and prevention could lead to healthism and fear-inducing perspectives about sex. Healthism is a social and cultural belief that implies that your physical, mental and sexual health is your own responsibility, turning the discourse with moral implicit judgments (and prejudices). The reality of matter is more complex than that and leaving the responsibility on a singular individual is just not fair. When you grow up in a society that does not include sex-ed, it’s more than comprehensible that you fall into mistakes and risks while experiencing your sexual relationships!
What is necessary to do is to admit there are people who still don’t use contraceptives or preventive methods and stay open and positive about it regardless, in order to create a safe and welcoming discourse on sexual health. It’s still possible to comprehend the context in which non-safe sex is made: because of wrong beliefs about pleasure (for example: for people with penises to not use the condom because “they don’t feel anything”) or because they do actually prefer it in that risky way. Leaving people their agency to choose is part of an inclusive CSE.
Concepts about safer sex mostly depend on where you live and how you grew up: information, discussions and beliefs can change whether or not you are in a propositional environment, where opportunities should be meant to be for everyone.
Finding information and getting support
Sexual health is to be treated as any other health issue. If you feel that there’s a lack of information about sex and health in your school, consider talking to your school administrators, teachers, or even your parents about the importance of comprehensive sex education.
In the absence of CSE in your school, consider seeking reliable online resources and books that provide information about sexual health, consent, and relationships. An online platform that can be of a great assistance, in terms of available resources is thegendertalk.eu/library/sex-ed-resource-database/
“When I went to the gynecologist, no one explained anything to me and they just explored me and that was all, without giving me any information.”
Going to see doctors is the best practice we can learn to keep ourselves healthy. However, sometimes it may become an uncomfortable or even a traumatic event, as unfortunately some doctors don’t provide us enough information and/or don’t ask us for consent to touch or explore our bodies for medical purposes. Still, we should always claim our right to bodily autonomy, which shall protect us from violent situations and that claims that we have dignity and agency of our own body and we should be able to make decisions over it.
On other occasions, visits to the doctor is the only time when we might receive some information concerning our sexuality. Nevertheless, the fact that we only learn about our sexuality when we go to the doctor (gynaecologist, urologist, sexual specialists, etc.) might make us believe that sexuality is strictly linked to our anatomy and, particularly, to our genitals and reproductive system. This makes us forget that sexuality is a really broad concept that also refers to our gender identity and sexual orientation, to our desire and pleasure, to the relationships we establish, to our self-esteem, and so on.
References
Center for Reproductive Rights (n.d). Last retrieved 4 February 2024 from https://reproductiverights.org/
Guerra J. (2019). Le donne etero hanno meno orgasmi di tutti. E la colpa è del sessismo. Last retrieved 4 February 2024 from https://thevision.com/attualita/orgasmo-donne-etero-sessismo/
Introduction to Puberty (n.d.). Teen Health Source. Last retrieved 4 February 2024 from https://teenhealthsource.com/puberty/introduction-puberty/
Merone L.,Komla T., Darren R. (2022). Sex Inequalities in Medical Research: A Systematic Scoping Review of the Literature. Womens Health Rep (New Rochelle). Last retrieved 4 February 2024 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8812498/
Palumbo J. (2022). The Body Positive Movement Encourages Inclusion, Not Obesity. Forbes. Last retrieved 4 February 2024 from https://www.forbes.com/sites/jenniferpalumbo/2022/05/12/how-the-body-positive-movement-doesnt-encourage-obesity-but-inclusion/
Planned Parenthood. (n.d.). Puberty. Last retrieved 4 February 2024 from https://www.plannedparenthood.org/learn/teens/puberty
STDs A to Z (n.d.). Last retrieved 4 February 2024 from https://www.ashasexualhealth.org/stds_a_to_z/
The World’s abortion laws. Center for Reproductive rights. Last retrieved 4 February 2024 from https://reproductiverights.org/maps/worlds-abortion-laws/
What is pleasure? (n.d.). Options for Sexual Health. Last retrieved 4 February 2024 from https://www.optionsforsexualhealth.org/facts/pleasure/
WHO. (2023). Endometriosis Key Facts. Last retrieved 4 February 2024 from https://www.who.int/news-room/fact-sheets/detail/endometriosis#:~:text=Overview,period%20and%20last%20until%20menopause
Liji T. (2022). The effects of continuous contraceptive pill taking. News-medical. Retrieved 21 February 2022 from https://www.news-medical.net/health/The-Effects-of-Continuous-Contraceptive-Pill-Taking.aspx#:~:text=There%20are%20two%20ways%20in,there%20are%20no%20withdrawal%20bleeds.
O’Connel H., Sanjeevan K.V., Hutson M. J (2005). Anatomy of the clitoris. Journal of Urology.